Best Navigating the Hysterectomy Surgery: A Guide to What to Expect
Hysterectomy is a significant health decision that has a tendency to elicit a response of feelings, from hope and relief to fear and disorientation. Whether due to the cause of the procedure—fibroid, endometwriosis, adenomyosis, uterine prolapse, cancer, or chronic pelvic pain—the awareness of what to expect will enable you to approach the procedure with greater ease and assurance. From initial consultation to road to recovery and after, this is a complete guide to walk you step by step through every stage of a hysterectomy, equipping you with information and useful advice to prepare you mentally, emotionally, and physically.
Getting to Grips with the Foundations of Hysterectomy Surgery
Hysterectomy is a surgical operation in which the uterus is cut out. The ovaries (oophorectomy), cervix, and fallopian tubes (salpingectomy) are excised by the surgeon depending on the patient's condition and the typical medical condition. To have complete information about the kind of hysterectomy suggested to you and the risks of losing these organs, you must consult all this with your gynaecologist thoroughly.
There are some surgical methods of having a Hysterectomy Surgery, each with its own advantages and implications:
Abdominal Hysterectomy: The traditional open incision in the lower belly. It is the best possible visibility for the surgeon and is most commonly done for large uteruses or cancer. It does generally mean longer recovery and a more visible scar, however.
Vaginal Hysterectomy: Uterus removal through incision inside the vagina. No external scar can be seen after surgery, and it generally allows for quicker recuperation than an abdominally performed hysterectomy. It is generally best suited for uterine prolapse or smaller uteri.
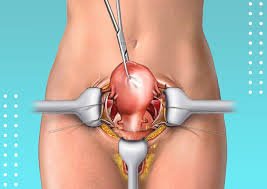
Laparoscopic Hysterectomy: It is a minimally invasive method in which multiple small incisions are made in the abdomen through which the surgeon introduces surgical instruments and a laparoscope—a thin, camera tube. The surgeon operates while viewing the site of operation on a video monitor. Laparoscopic hysterectomy usually leaves smaller scars, less pain, and quicker recovery than abdominal hysterectomy.
Robotic-Assisted Laparoscopic Hysterectomy: A type of laparoscopic surgery where the robot is used to perform with robotic arms to manipulate the instruments more precisely, dexterously, and visually. Benefits are similar to traditional laparoscopic surgery.
Your doctor will discuss the most appropriate technique based on your individual condition and medical history. Don't hesitate to ask about risks, advantages, and rehabilitation for each.
Preparation for Your Hysterectomy Surgery
Preparation is the key to easier surgery and recovery. The following are some of the steps that you can carry out:
Medical Evaluation and Clearance: Your physician will do a physical examination, a medical history, order blood work, imaging studies (e.g., ultrasound or MRI), and an electrocardiogram (ECG) to evaluate you in its entirety and to make sure that you are a good candidate for surgery.
Discuss Medications and Supplements: Tell your doctor about all the medications you take, including over-the-counter, prescription, herbs, and vitamins. Certain drugs, including blood thinners, will have to be discontinued several days prior to surgery.
Lifestyle Adjustments: You need to quit smoking several weeks prior to your surgery since it delays recovery and increases the risk of complications. Your overall success of your surgery also is augmented by healthy diet and healthy weight. Mild exercise each day as tolerated will make you fitter.
Pre-operative preparation: Bathing or showering with antiseptic soap, fasting (for how long before surgery you should avoid food and fluids), and additional preparations you will be asked to do will be explained in detail by your surgery team.
Post-Operative Care Plan: For your initial recuperation time, make arrangements for someone to take you home from the hospital and help out with childcare, housework, and pet care. Having someone to help will make your recuperation a lot less stressful.
Prepare Your Home: Plan a restful recuperation area in your home. This can include setting up pillows to support you, having things you need most easily accessible, and having warm clothing and entertainment supplies available.
Cope with Emotional Problems: Nervousness or anxiety before surgery is natural. Talk over your feelings with a family member or close friend, your physician, or a counselor. To connect with other women who have undergone hysterectomies, investigate a support group.
What to Expect on the Day of Hysterectomy Surgery
You will visit the hospital in the morning of your surgery and perform the pre-operative protocol that is needed, such as an interview with the anaesthesiologist, dressing up in a hospital gown, and being escorted for your vital signs. The anaesthesiologist will answer any questions that you have and discuss the type of anaesthesia that you will be given, which is most commonly general anaesthesia, which renders you unconscious.
Surgery duration will vary with the kind of hysterectomy performed and the case's complexity. You will be transferred to the recovery room afterwards, where you will be monitored as you wake up from anaesthesia. You will be administered pain medication, anti-vomiting prevention, and prevention of grogginess medication.
You will then be transferred to a hospital room once you stabilize. For how long you will remain in the hospital, usually one to several days, also depends on what surgery you had and how well you're otherwise recovering. Your pain will be watched over by the doctors and nurses while you are in the hospital, checked to see if you are able to tolerate foods and liquids, and you will be prompted to move around as much as possible in an attempt to get the circulation moving and avoid complications.
Conquering the Recovery Period
The recovery period after a hysterectomy is crucial for healing and regaining your strength. It's essential to follow your doctor's instructions carefully and allow your body ample time to recover.
Pain Relief: You will likely have some discomfort and pain after surgery. Your surgeon will give you medication to help with this. Take the medication as instructed and don't wait until the pain is quite severe before taking the medication.
Wound Care: If you've had an abdominal or laparoscopic hysterectomy, you will have incisions that need to be dried and cleaned. Bathe or shower as instructed by your doctor and watch for signs of infection like greater redness, swelling, drainage, or fever. When a vaginal hysterectomy is performed, there might be some vaginal bleeding or discharge, which is normal but should subside over a period of time.
Rest and Activity: Good rest is important for recovery. Steer clear of heavy exercise, heavy lifting (more than 10 pounds), and long periods of standing or sitting for a few weeks. Your physician will instruct you on gradually going back to normal activities. Walking is frequently recommended shortly after surgery in an effort to maintain the circulation and prevent blood clots.
Diet and Fluids: Follow a good balanced diet with adequate fruits, vegetables, and fiber to prevent constipation, which is a frequent complaint following surgery because of pain medication and limitation of movement. Maintain adequate fluid intake.
Emotional Well-being: It is not unusual to feel a variety of emotions when recovering, such as sadness, tiredness, and even hormonal shifts if your ovaries were removed. Be kind to yourself and ask the support of your loved one or counselor if necessary.
Follow-Up Visits: You will come back for follow-up visits with your physician to check on the progress of your recovery as well as to deal with any problems. Be sure to keep all follow-up visits and ask questions that you have.
Long-Term Prognosis After Hysterectomy Procedure
For most women, a hysterectomy procedure can greatly enhance their quality of life by eliminating pain, heavy bleeding, and other disabling symptoms. However, care must be taken about the possible long-term consequences, particularly if the ovaries were also removed.
Hormonal Changes: If you underwent removal of your ovaries (oophorectomy), you will undergo surgical menopause, and that might cause symptoms like hot flashes, night sweats, vaginal dryness, and mood swings. Your doctor may talk to you about hormone replacement therapy (HRT) to treat these symptoms.
Pelvic Floor Health: Hysterectomy surgery occasionally involves changes in pelvic floor muscles. Doing Kegel exercises will make those muscles stronger and avoid problems like urinary incontinence.
Sexual Health: While some women may feel change in sex desire or feeling after hysterectomy surgery, the majority of them say their sex life improves due to relief from prior discomforts. Discussing openly with your partner is essential.
Emotional Adjustment: Adjustment to Hysterectomy Surgery is a personal experience. Some will feel a sense of loss or grief, others a feeling of liberation. Give yourself a little time to work through your feelings and refer if necessary.
Empowering Yourself Through Knowledge
.jpg)
.jpg)
.jpg)
Comments
Post a Comment